Rectal Prolapse: Introduction, Clinical features, Diagnosis, Management: Surgery
Hellow guys, Welcome to my website, and you are watching Rectal Prolapse: Introduction, Clinical features, Diagnosis, Management: Surgery. and this vIdeo is uploaded by Dr.G Bhanu Prakash Animated Medical Videos at 2024-09-25T07:49:59-07:00. We are pramote this video only for entertainment and educational perpose only. So, I hop you like our website.
Info About This Video
| Name |
Rectal Prolapse: Introduction, Clinical features, Diagnosis, Management: Surgery |
| Video Uploader |
Video From Dr.G Bhanu Prakash Animated Medical Videos |
| Upload Date |
This Video Uploaded At 25-09-2024 14:49:59 |
| Video Discription |
📌 𝐅𝐨𝐥𝐥𝐨𝐰 𝐨𝐧 𝐈𝐧𝐬𝐭𝐚𝐠𝐫𝐚𝐦:- https://www.instagram.com/drgbhanuprakash
📌𝗝𝗼𝗶𝗻 𝗢𝘂𝗿 𝗧𝗲𝗹𝗲𝗴𝗿𝗮𝗺 𝗖𝗵𝗮𝗻𝗻𝗲𝗹 𝗛𝗲𝗿𝗲:- https://t.me/bhanuprakashdr
📌𝗦𝘂𝗯𝘀𝗰𝗿𝗶𝗯𝗲 𝗧𝗼 𝗠𝘆 𝗠𝗮𝗶𝗹𝗶𝗻𝗴 𝗟𝗶𝘀𝘁:- https://linktr.ee/DrGBhanuprakash
Rectal Prolapse: Introduction, Clinical features, Diagnosis, Management: Surgery -
-------------------------------------------------------------------------------------------------------------------
Clinical Features -
The clinical features of rectal prolapse vary depending on the severity and duration of the condition:
Visible Protrusion:
Patients may notice a bulging mass coming out of the anus, especially after defecation.
In complete prolapse, the entire rectal wall may protrude, while in partial prolapse, only the mucosa is visible.
Pain or Discomfort:There may be discomfort or pain in the rectal region, especially during bowel movements.
The prolapsed rectum may cause a dragging sensation.
Rectal Bleeding:Due to mucosal irritation and trauma, bleeding may occur, often accompanied by mucous discharge.
Fecal Incontinence:Loss of bowel control is common, especially with complete prolapse.
This can be socially embarrassing and significantly affect the patient’s quality of life.
Constipation:Some patients develop chronic constipation due to rectal prolapse.
There may be a need to manually push the prolapse back in to complete defecation.
Straining:Chronic straining during bowel movements can both cause and exacerbate rectal prolapse.
Diagnosis :
Diagnosis of rectal prolapse is generally clinical, but specific investigations can help assess the extent and severity of the condition.
Physical Examination:
A thorough inspection of the perineum can often confirm the diagnosis.
The patient may be asked to strain (Valsalva maneuver) to visualize the prolapse.
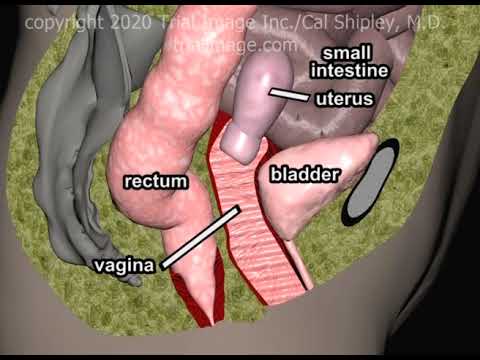
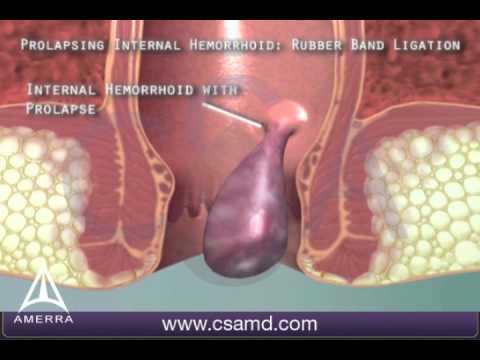
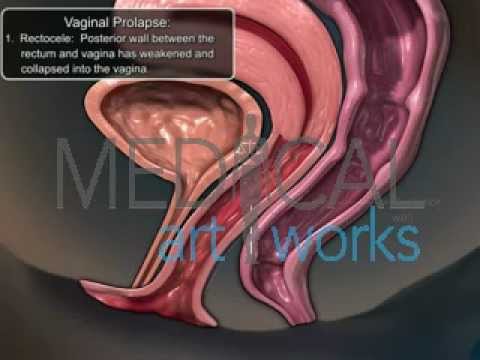
Digital Rectal Examination (DRE):To assess the tone of the anal sphincter and detect any other associated conditions like internal hemorrhoids or rectocele.
Defecography:A specialized X-ray or MRI where the patient is asked to defecate a contrast material.
It provides insight into the pelvic floor anatomy and prolapse severity.
Colonoscopy:Used to rule out polyps, tumors, or other lesions in the rectum or colon, particularly in older patients with associated rectal bleeding.
Anal Manometry:This measures anal sphincter pressure, which can be useful in patients with incontinence.
Management: Surgical and Non-Surgical
Non-Surgical Management
Dietary Modifications:High-fiber diet and hydration to prevent constipation and reduce straining during defecation.
Pelvic Floor Exercises:Kegel exercises can help strengthen the pelvic muscles and reduce the risk of prolapse worsening.
Stool Softeners or Laxatives:These help in ensuring smooth bowel movements without straining.
Manual Reduction:In some cases, patients can manually push the prolapse back into place.
Surgical Management -
Surgery is the definitive treatment for rectal prolapse, especially in patients where the prolapse is severe, recurrent, or associated with fecal incontinence.
1. Perineal Procedures:
Perineal Rectosigmoidectomy (Altemeier Procedure):This involves the removal of the prolapsed segment via the perineum and is often performed in elderly patients or those unfit for major surgery.
Delorme Procedure:In this technique, the mucosal layer of the prolapsed rectum is removed, and the muscular layer is plicated (folded) to tighten the prolapsed rectum.
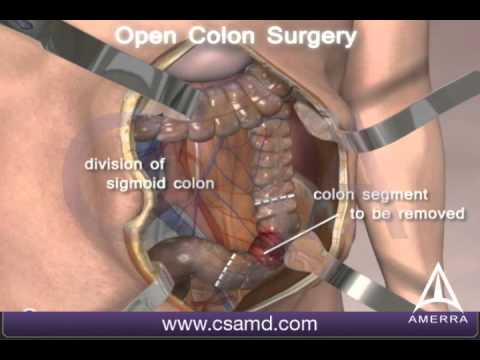
2. Abdominal Procedures:
Rectopexy:Involves the repositioning and fixation of the rectum to the sacrum or pelvic wall to prevent further prolapse. This can be done via laparoscopy or open surgery.
Sometimes, a mesh is used to reinforce the attachment.
Resection Rectopexy:Combines the resection of redundant bowel and fixation of the rectum. This is often used in patients with coexisting constipation.
3. Laparoscopic Surgery:Minimally invasive surgery with laparoscopic rectopexy or laparoscopic sigmoid resection is increasingly preferred due to quicker recovery times and fewer complications.
Postoperative Care:Avoid heavy lifting or straining for several weeks.
Pelvic floor physiotherapy may be recommended to strengthen the muscles after surgery.
Stool softeners or laxatives may be continued to avoid constipation.
#RectalProlapse #ProlapseSurgery #PelvicFloorHealth #RectalHealth #ProlapseTreatment #SurgeryAwareness #ColorectalSurgery #PelvicDisorders #Healthcare #BowelHealth #SurgicalManagement
#medicalanimations #fmge #fmgevideos #rapidrevisionfmge #fmge2024 #mbbslectures #nationalexitexam #nationalexittest #neetpg #usmlepreparation #usmlestep1 #fmge #usmle #drgbhanuprakash #medicalstudents #medicalstudent #medicalcollege #neetpg2025 #usmleprep #usmlevideos #usmlestep1videos #medicalstudents #neetpgvideos #usmlestep2videos |
| Category |
Education |
| Tags |
rectal prolapse | rectal prolapse surgery | signs rectal prolapse | rectal prolapse symptoms | treatment options rectal prolapse | rectal prolapse treatment | symptoms rectal prolapse | rectal prolapse causes | rectal prolapse cure | clinical features of rectal prolapse | diagnosis of rectal prolapse | rectal prolapse management | rectal prolapse usmle step 1 | rectal prolapse usmle | rectal prolapse neetpg | common symptoms rectal prolapse | rectal prolapse treatment usmle | usmle step 1 | NMC |
More Videos

.png)